The role of HEOR in the assessment of drug pricing and reimbursement policies
- 1 HEOR Components in Drug Pricing and Reimbursement
- 2 HEOR challenges and limitations in drug pricing and reimbursement
- 2.1 The subjectivity of evaluation
- 2.2 Insufficient data
- 2.3 Need for data updates
- 2.4 Impact on Decisions by insurance companies and the Government
- 2.5 Lack of patient participation
- 2.6 Non-transparent data
- 2.7 Restrictions on the use of certain methods
- 3 HEOR in Drug Pricing and Reimbursement
- 4 Conclusion
In many countries, governments and health insurers are taking action to influence the price and use of medicines in order to promote their effectiveness and cost-effectiveness. One important factor influencing pricing and reimbursement decisions for medical technologies, including drugs, is economic evaluation, which offers a method for assessing the added value of new medical interventions to society compared to existing treatments.
HEOR, or Health and Economic Evaluation Research, is an important tool used in health systems to evaluate the clinical and economic effectiveness of medications. The use of data from HEOR studies can inform pricing and reimbursement decisions about medications.
HEOR Components in Drug Pricing and Reimbursement

HEOR is an area of research that evaluates the clinical and cost-effectiveness of medical technologies and drugs, and their impact on patient health outcomes.
Learn more about health economics outcomes research.
Clinical Outcomes
One area of HEOR research is evaluating the effectiveness and safety of medical technologies through clinical trials and other research methods. It includes:
- examining the effects of a drug on a disease
- mortality;
- quality of life.
The types of studies used to study clinical outcomes are:
- clinical trials (phase I-IV);
- meta-analysis;
- retrospective and prospective studies;
- registry and database studies.
Evaluation of the effectiveness of medical technologies relies on clinical outcomes to assess the possible clinical benefits and risks of using drugs and other medical technologies, as well as to determine their place in comparison with existing therapies.
Economic Outcomes
HEOR also assesses the cost-effectiveness of medical technologies and drugs by analyzing costs, outcomes, and comparing their ratios. The evaluation includes:
- drug costs;
- economic benefits;
- costs of other medical services.
The types of studies most often conducted to assess cost-effectiveness are:
- economic modeling;
- cost-effectiveness analysis;
- cost-benefit analysis;
- assessing the budgetary impact of new medical technologies.
Economic outcomes are one of the key components of healthcare costing studies that influence drug pricing and reimbursement policies. They provide an estimate of the cost-effectiveness of medical technologies, allowing us to assess the cost of introducing new technologies into the healthcare system and their impact on costs and treatment outcomes.
Economic outcomes assessments are an important tool for drug pricing and reimbursement decisions because they:
- can assess the cost and effectiveness of drug technologies by comparing them to other alternatives;
- can help determine optimal pricing strategies, including determining the optimal drug price that is fair and sustainable for the health care system, patients, and drug manufacturers.
Economic results can also inform drug reimbursement decisions, allowing the fiscal impact to be assessed and determine which drugs will be included in insurance programs or publicly funded. This allows for more efficient use of limited resources in health care and ensures that drugs are available to patients who need treatment.
Patient-reported outcomes
These studies aim to examine patients’ perceptions and experiences with medical technologies, and assess their effects on patient health and life.
Studies conducted to examine patient-reported outcomes may include:
- surveys;
- interviews;
- focus groups;
- other data collection methods that allow patients to express their opinions, assess their health status, and evaluate the effects of medications on their quality of life and daily tasks.
The importance of such studies for drug pricing and reimbursement decisions is that they allow patients’ opinions and assessments to be taken into account, which is important for developing patient-driven health policies and achieving optimal treatment outcomes.
Patient-reported outcomes can be used to assess the value of medications and their alignment with patient expectations and preferences. These data can influence medication pricing decisions and reimbursement decisions because they can help assess the relationship between medication costs and patient benefits, as well as the development of recommendations for medication use in actual clinical practice, which affects the extent to which they are reimbursed by insurance companies and government agencies.
Assessing patient-reported outcomes can also help prioritize resources and develop effective payment mechanisms for medications, taking into account patient preferences and needs.
HEOR challenges and limitations in drug pricing and reimbursement
Although HEOR is an important component of health care, there are some problems and limitations of this tool that should be considered:
The subjectivity of evaluation
Estimating cost-effectiveness and treatment outcomes is often subjective and can depend on the methodologies and assumptions used. New HEOR techniques to improve evaluation, such as the use of artificial intelligence, can help improve estimates of treatment effectiveness and reduce their subjectivity.
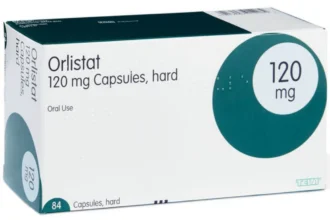
Insufficient data
HEOR analysis requires sufficient data, which may be limited in some cases. For example, to estimate the life expectancy of patients with a particular disease, it is necessary to have access to long-term clinical studies, which can be difficult. Additional data can be obtained by conducting new clinical trials.
Need for data updates
Drug efficacy can change over time, so data on cost-effectiveness and treatment outcomes must be continually updated.
Impact on Decisions by insurance companies and the Government
Drug prices and reimbursement decisions can influence insurance companies and government decisions. However, such decisions can be biased, which can have a negative impact on patients. Therefore, decisions about drug pricing and reimbursement must be made in close collaboration among all stakeholders, including patients, drug manufacturers, insurance companies, and government agencies. Dialogue and compromise can help find fairer and more effective solutions.
Lack of patient participation
HEOR evaluates treatment effectiveness based on patient data, but sometimes does not consider patients’ opinions and preferences.
Non-transparent data
In some cases, data on cost-effectiveness and treatment outcomes are not publicly available, which can make evaluation difficult.
Restrictions on the use of certain methods
Some countries have restrictions on the use of some HEOR methods, which may limit the ability to estimate cost-effectiveness of treatment.
HEOR in Drug Pricing and Reimbursement
An example of the use of HEOR methods in drug pricing and reimbursement can be seen in the Affordable Medicines Reimbursement Program framework and impact assessment in Ukraine.
In 2017, the Ukrainian government launched the Affordable Medicines Program (AMP), designed to reimburse prescription drugs in outpatient settings. Despite the clear benefits of the program, it is important to examine its design to identify current trends, strengths, and weaknesses that can be used to support its further improvement and development of reimbursement models. The purpose of this study was to assess which AMP pricing strategies might affect the potential for providing patients with affordable medications.
The analysis of the AMP system included an assessment of several parameters, such as pricing mechanisms, drug manufacturers, volume of drugs covered by the program, and volume of consumption. Data were obtained from official government databases and public sources, and statistical methods were used for analysis.
The results of the study showed that from 2017 to 2021, the AMP system showed significant growth in the number of covered drugs, consumption volumes, and reimbursable international nonproprietary names. The pricing constraints applied to the AMP structure were proportional to the number of manufacturers involved in the program. At the same time, the number of drugs containing reimbursable international nonproprietary names, but not included in the program, was decreasing.
From the study’s findings, the AMP structure has a significant impact on the pharmaceutical market and the ability to provide patients with a wide range of drugs while effectively managing state and patient health care costs. However, a tool is needed to re-evaluate AMPs to allow for timely identification of deficiencies, evaluation of effectiveness, and to facilitate targeted development in accordance with pharmaceutical market trends and achievement of desired patient health outcomes.
Conclusion
HEOR plays an important role in drug pricing and reimbursement decisions by evaluating the effectiveness of drugs and their impact on patient health. The use of HEOR data in decision-making can improve healthcare quality and optimize drug costs. In the future, HEOR development can help shape more accurate and effective evidence-based, patient-centered drug pricing and reimbursement policies.