What Conditions Qualify for TPD Insurance Claims?
- 1 What TPD Insurance Means in Australia
- 1.1 Policy Definitions That Determine Eligibility
- 1.2 Physical Conditions That Generally Qualify
- 1.3 Mental Health and TPD Claims
- 1.4 Commonly Disputed Conditions
- 1.5 Building Strong Medical Evidence
- 1.6 Practical Steps for Claim Success
- 1.7 When Claims Are Denied
- 2 Conclusion
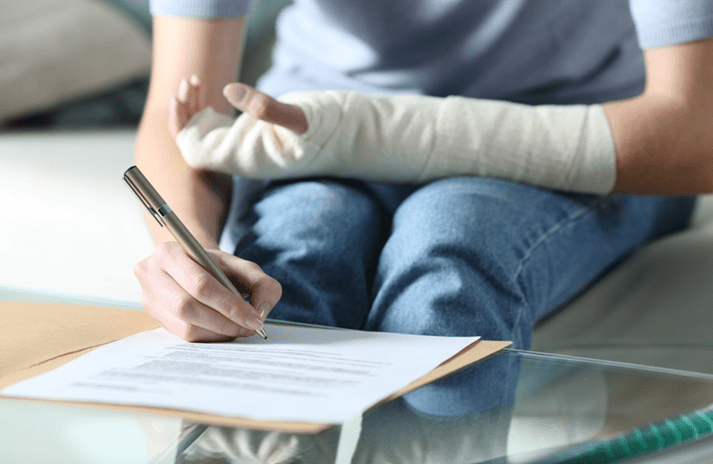
Navigating the complex world of insurance claims can be overwhelming, especially when you’re dealing with a serious medical condition that affects your ability to work. If you’re considering making a Total and Permanent Disability (TPD) claim, understanding which conditions qualify is essential. Seeking advice from experienced TPD lawyers in Newcastle can make a significant difference to the success of your claim and the compensation you receive.
- TPD claims are assessed based on policy definitions (own occupation, any occupation, or activities of daily living)
- Physical injuries, neurological disorders, organ failure, and mental health conditions may qualify depending on severity.
- The strength of medical evidence and documentation is crucial to claim success.s
- Chronic pain and conditions without objective tests are commonly disputed
- Professional legal support can significantly improve claim outcomes
What TPD Insurance Means in Australia
Total and Permanent Disability (TPD) insurance provides financial protection if you become permanently unable to work due to illness or injury. Most Australians hold TPD cover through their superannuation funds, while others have standalone retail policies or group coverage provided by their employers.
TPD claims typically take 6-12 months to process, with successful claims resulting in lump-sum payments that can range from tens of thousands to over a million dollars, depending on your policy and circumstances.
Policy Definitions That Determine Eligibility
The specific wording in your policy directly impacts which conditions qualify for a TPD claim. There are three main definitions insurers use:
- Own occupation: You cannot perform your specific job or profession (most favourable to claimants)
- Any occupation: You cannot work in any job suited to your education, training, or experience
- Activities of daily living: You cannot perform basic self-care tasks (strictest definition)
Policy wording variations can dramatically affect eligibility. For example, some policies require you to be “unlikely to ever” return to work, while others use “unable to ever” return to work – a subtle but important distinction.
Physical Conditions That Generally Qualify
Certain serious physical conditions typically have higher approval rates for TPD claims:
Major physical injuries: Severe spinal cord injuries resulting in paraplegia or quadriplegia, traumatic amputations of limbs, and catastrophic brain injuries often qualify.
Advanced neurological disorders: Conditions such as motor neurone disease, multiple sclerosis (advanced stages), Parkinson’s disease, and stroke with significant permanent disability frequently meet the threshold.
End-stage organ failure: Terminal conditions like advanced heart failure, end-stage renal disease requiring dialysis, or respiratory failure needing continuous oxygen therapy typically qualify.
The severity of the condition itself isn’t always the determining factor. What matters most is how the condition impacts your ability to work within the specific terms of your policy definition. – Conrad Curry
Mental Health and TPD Claims
Mental health conditions can qualify for TPD benefits, though these claims often face greater scrutiny:
Insurers typically consider severe and persistent psychiatric conditions, including major depression, PTSD, bipolar disorder, and schizophrenia, when there’s evidence of significant functional impact despite appropriate treatment.
Successful mental health claims generally require:
- Comprehensive psychiatric reports from treating specialists
- Evidence of consistent, long-term treatment (medication, therapy)
- Detailed documentation of functional limitations
- Proof that all reasonable treatment options have been exhausted
Commonly Disputed Conditions
Some conditions face higher rates of claim disputes and denials:
Chronic pain syndromes: Conditions like fibromyalgia and chronic fatigue syndrome often meet resistance as they rely heavily on self-reported symptoms with limited objective testing.
Soft tissue injuries: Back injuries, whiplash, and repetitive strain injuries may be challenged if imaging results don’t align with reported disability levels.
Pre-existing conditions: Claims may be rejected if there’s evidence you had the condition before taking out the policy, particularly if it wasn’t disclosed.
Building Strong Medical Evidence
Insurers assess claims based on multiple sources of medical evidence:
Treating doctor reports carry significant weight, particularly when they include detailed functional assessments rather than just diagnoses. Specialist opinions that specifically address your inability to work according to policy definitions are particularly valuable.
Insurers often arrange independent medical examinations (IMEs) to verify your condition. Understanding that these doctors work for the insurer and preparing accordingly can help strengthen your claim.
Functional capacity evaluations provide objective evidence of your physical limitations and are particularly useful for physical injury claims.
Practical Steps for Claim Success
To maximise your chances of TPD claim approval:
Review your policy thoroughly to understand exactly which definition applies to your situation. Collect comprehensive medical documentation, including test results, specialist reports, and treatment records spanning your entire medical journey.
Maintain a detailed diary of your symptoms and limitations to demonstrate consistency in your reported disability. Ensure your doctors understand the specific policy requirements when they prepare supporting documentation.
Be mindful of social media activity, as insurers often monitor these platforms for evidence that contradicts your claimed limitations.
When Claims Are Denied
If your claim is rejected, you have several options:
Begin with the insurer’s internal dispute resolution process, clearly addressing the specific reasons for denial. If unsuccessful, you can escalate to the Australian Financial Complaints Authority (AFCA) for free external dispute resolution.
For complex or high-value claims, legal action may be necessary. This typically involves gathering additional expert evidence and preparing for a more formal process.
Conclusion
The success of a TPD claim largely depends on how your specific condition aligns with your policy definition and the quality of evidence supporting your inability to work. While severe physical conditions often have clearer pathways to approval, mental health and chronic pain conditions can also qualify with proper documentation and expert support.
If you’re struggling with a serious medical condition that prevents you from working, don’t attempt to navigate the complex TPD claim process alone. Conrad Curry can provide the expertise needed to assess your eligibility, gather appropriate evidence, and present your claim in the strongest possible light.